ICSI - the exquisite tool in IVF
History of IVF with ICSI for Infertility
By Dr. Joe Massey, MD
The early years
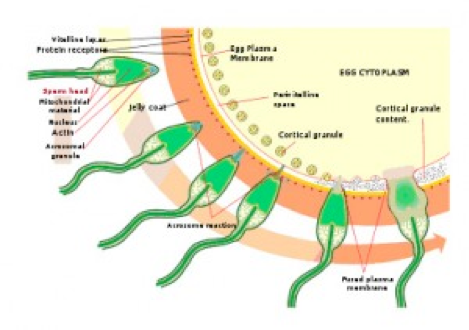
In the early years of IVF treatment, eggs often failed to fertilize when mixed with sperm from men with low sperm counts. In some cases, all went well. But in others, the sperm were not only low in number, but also failed to penetrate the zona pellucida (shell around the egg) due to disorders of the function of the sperm. It seemed like if the sperm were right in the dish, they coundn’t miss – but they did.
Investigators in IVF labs used a variety of methods to breach the zona, making it easier for sperm to enter. The puzzle was that once a hole was made, the block to polyspermy (more than one sperm entering an egg) was lost and extra sperm would enter. Thus, these attempts did not consistently improve pregnancy rates.
Early advances
In the mid 1980s, embryologists at Reproductive Biology Associates (RBA) in Atlanta were attempting to alleviate this frustration. Drs. Henry Malter and Jacques Cohen spearheaded an approach called partial zona dissection (PZD), which used a needle to cut an angled slit in the zona. This strategy allowed limited numbers of sperm to enter. The sperm were in the dish, still required to “find” the egg. Then the problem became an overabundance of sperm slipping into this slit, and polyspermy was still frequent. PZD offered some improvement in male factor IVF, but no one was satisfied with the outcomes.
Intracytoplamic sperm injection (ICSI) had been tried in humans but failed and was pronounced untenable despite having been successful in a variety of animals. It was not until 1992 that a group in Belgium led by DG Palermo and Andre van Sterteghem solved the puzzle first. Once safety and efficacy were illustrated, ICSI was reported as practical in humans and was rapidly adopted all over the world. RBA was at the forefront of this technological advance and became the first IVF program in the U.S. to achieve a pregnancy and birth through ICSI.
There are several hundred publications related to the past and current efforts to improve male factor outcomes in IVF with ICSI. Now, thanks to continuing improvements, the male factor infertility diagnostic group of patients have the same fertilization take-home-baby rates as those in other diagnostic groups.
ICSI for male infertility
Men with low sperm parameters should first have an evaluation to determine cause of the problem. Sometimes correction is possible, but often the path of least resistance is to move directly to IVF with ICSI.
Men who are trying to conceive without success who have low numbers of sperm present, low motility, or abnormal sperm shapes are the primary candidates for ICSI. The shapes of the sperm are now classified by strict microscopic criteria. To be declared normal, the shape of the sperm must be perfect.
The Kruger morphology is the criteria for normal semen analysis, which is reported by your IVF lab. If the percent of sperm that are normal by these criteria is under 4%, the man is a candidate for ICSI.
Minor defects in the shape of the head are associated with genetic defects. Andrology specialists in IVF labs make these determinations looking at the fixed sperm under high magnification.
Special screening
In severe male factor infertility, under 5 million/cc, there is an increased risk that there is a genetic abnormality. About 5% of this category of men will have a genetic error detected. Since some of these errors can result in miscarriage or affected children, men in the severe male infertililty category are ideally screened with a chromosome assay before beginning the IVF with ICSI process.
Optionally, screening can be done for another minor genetic defect, the DAZ gene deletion. If this deletion is the cause of the infertility, ICSI can result in a male child with the same deletion and resulting infertility.
ICSI is used broadly
Because failed fertilization is a threat in any case of unexplained infertility, IVF with ICSI is often used on half of all the eggs in a first IVF cycle. As mentioned earlier, some centers use ICSI in every case. Other experts decry this approach as unnecessary.
- If any IVF cycle results in failed or low fertilization, ICSI is used subsequently.
- If any IVF cycle results in failed or low fertilization, ICSI is used subsequently.
- If you plan to use preimplantation genetic diagnosis after embryos develop, ICSI is used for the fertilization to make certain that only one sperm provides genetic material to the embryo.
- If you plan to use preimplantation genetic diagnosis after embryos develop, ICSI is used for the fertilization to make certain that only one sperm provides genetic material to the embryo.
The good news is that as long as the sperm are alive, ICSI can provide fertilization and embryo development approaching that of men with normal sperm, i.e. 70% to 80%.
How does ICSI work?
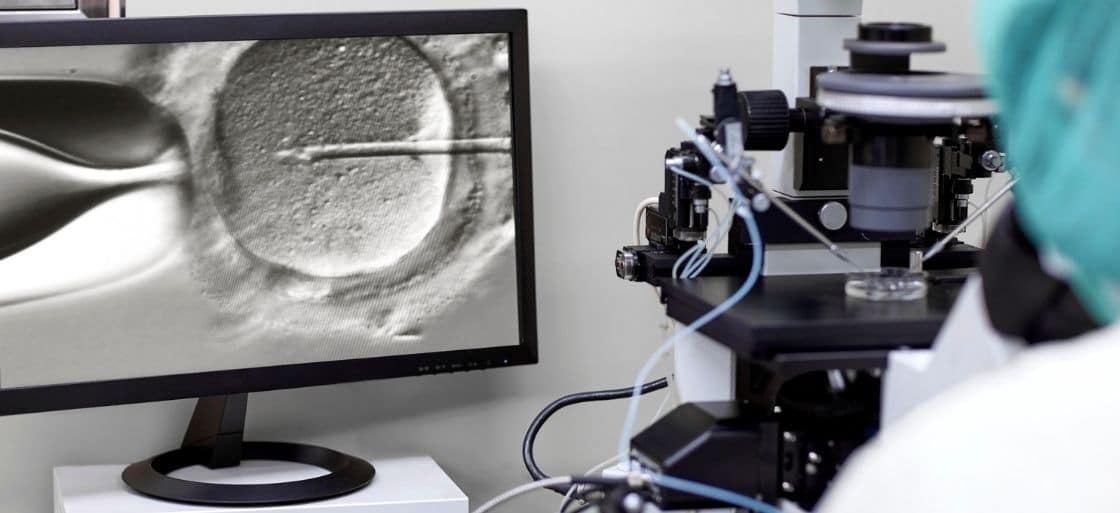
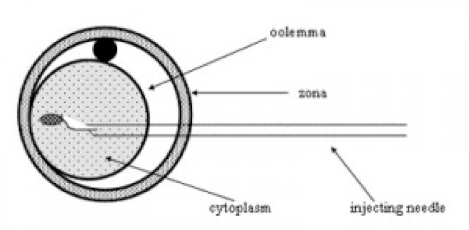
Like using angel hair to puncture a speck of dust, ICSI is an amazing procedure. Injecting the egg, which is 80 microns in diameter (barely visible), with a sperm which is 100 times smaller requires a sophisticated micoromanipulation setup. These techiniques were a part of the science of cell biology for decades before IVF scientists began using them.
The precision device is set on a large base, which prevents vibrations from people walking around on the the surrounding floor. It allows manipulation of the sperm and eggs with joysticks gearing delicate movements down to the microscopic level. Highly trained embryologists master this technique and can inject several eggs in a half hour using the following process:
- Soon after retrieval, an egg is selected after the cumulus is stripped away by a chemical, allowing close observation of each egg for maturity. Immature eggs cannot succeed.
- Once the egg is stabilized with a suction pipette, the most perfect-appearing sperm is selected nearby, as it will have less chance of being chromosomally abnormal. The egg is held with a suction pipette, and the sperm is introduced with the tiny needle.
- The zona and egg are breached with another infinitesimal needle, the key to avoiding making an injurious large hole in the egg.
Causes of male infertility treatable by ICSI
Male infertility may be due to a variety of issues. Unfortunately, the most common category of male factor issues is “unexplained.” Despite all the years of research into the intricasies of sperm production and function, medical science simply cannot always diagnose the cause. We will touch on a few known conditions, though they may not provide a solution to your male factor problem. Because ICSI allows bypass of the cause of the problem with such success, the cause of male fertility problems becomes moot. Around 97% of the time, IVF with ICSI succeeds in fertilization, no matter the cause of male factor infertility.
Azoospermia
Men who ejaculate no sperm in the seminal fluid fit into one of two categories: those with and without obstruction in the anatomy. An easily diagnosed group of men have blockages of sperm due to congenital absence of the vas deferens, the tube leading sperm from the testis to the penis. Needle aspiration or surgical intervention allows retrieval of hundreds of sperm and this will be enough for IVF with ICSI. Men who have had vasectomy have the same option, also.
More difficult cases are those who have non-obstructive low sperm production. Most of them fit into the unexplained category. The number of sperm produced by their testis may be low, even though the other cells which produce testosterone are normal.
TESE
In the most severe cases, sperm has not been ejaculated. ICSI can succeed in many of these non-obstructive cases through a delicate surgery called Testicular Sperm Extraction (TESE), performed by experienced reproductive specialists. However, this procedure has a significant failure rate. Because the risk of failure to retrieve sperm with TESE is 40% to 60%, many men opt to have donor sperm available at the time of egg retrieval to assure that embryos will be available.
There is a small group of men who have been born with genetic issues which profoundly effect testosterone and sperm production. They produce no sperm and most of them will need sperm donors.
Why doesn’t ICSI work every time?
Human reproduction is inefficient. Fertilization, of course, must be followed by embryo development.
The egg may look perfect under the microscope but it’s what you can’t see that counts. Getting though the first day in ICSI when the eggs begin to show evidence of fertilization isn’t the entire battle. It’s not just the sperm that set the stage for further development; the egg can also be the cause of failed development. Five or six more days of progress are needed to get to the blastocyst stage, ready for implantation.
The more we know about fertilization and its complexities, we can see the many opportunities for one critical piece of the puzzle to fail to fall into place. ICSI bypasses some of the potential problems but it is still imperfect. Let’s look at some of the issues.
Egg factors and IVF failure
Chromosomal errors
Fertilization may occur, but the embryo may arrest in development if there is a major genetic error in the nucleus of the egg. The egg may have an abnormal complement of chromosomes and basically stops before the development process begins. Often the embryos will arrest at the four-to-eight cell stage. Around half the time, abnormal genetic complement in the egg before the sperm even arrives is actually the problem.
The only way to know if this is occurring is to wait for the blastocyst, perform embryo biopsy, and freeze the embryos. Chromosome analysis can be performed on a few cells from the embryo. This giant leap in IVF technology, called preimplantation genetic testing (PGT), allows selection of only chromosomally normal embryos for transfer.
Cytoplasm
If the cytoplasm of the egg, called the ooplasm, has not matured, cell division will fail somewhere in the fertilization or early development process. Subtle defects in the ooplasm may lead to arrest at any stage of development, leading to attrition of embryos in the days after the initial IVF regardless of ICSI. Out of seven fertilized eggs, you may have two to three embryos by the fifth or sixth day, when they are ready for implantation. Of course, there is a range of possible outcomes.
Key to successful development is the complement of mitochondria. Older women have fewer of these energy-producing organelles than ideal. We can’t diagnose this problem, but we know it is one of our barriers to success.
Sperm factors in ICSI failure
Genetic
Although uncommon, some men who have normal genes themselves have abnormally high numbers of genetically abnormal sperm. It’s frustrating to know this problem can exist when there is not a useful way to predict it or know that it happened.
DNA Fragmentation
There are commercial tests for the integrity of the DNA of the sperm. Your doctor may order this test. Though not universally accepted as valid, some centers use DNA fragmentation tests to investigate men who have normal-appearing sperm, but continue to fail when they are trying to conceive naturally.
Male infertility research has unveiled other issues
There is a population of men who fail to fertilize even with ICSI due to defects in sperm that experts are still not able to detect. Fortunately, total failure only occurrs in 3% of men. There are ongoing experiments to allow IVF to succeed even in these cases.
It’s not true when people say male fertility is overlooked in research. Much sophisticated basic science is being done with possible application for future patients. Let’s explore a few of the frontiers of male infertility abnormalities. Thankfully again, ICSI allows bypass of these problems.
Abnormalities of the centrosome
A critical role in the spatial management of chromosomes in humans is played by the tiny tubules of the centrosome, which is introduced from the midpiece of the sperm. This delicate organelle must function perfectly for the chromosomes to organize for cell division. If not perfectly lining up the genes, the embryo may arrest at an early stage. Unfortunately, this is an unpredictable defect.
There are some cases in which even ICSI fails to fertilize the eggs. It may take another generation of basic science to continue unlock applications of what is known to improve IVF for male infertility.
Sperm RNA
RNA, which was identified in sperm by researchers in 2011, also has a role in fertilization. Testing for the presence of normal RNA has been developed experimentally, suggesting a future means to diagnose some men with otherwise unexplained infertility.
PLC zeta
Recently theories revolve around the absence of PLC zeta protein. Reproductive scientists dream that future IVF labs might inject some of this protein at the time of ICSI.
ICSI: is it safe?
Since the sperm selection process is bypassed in ICSI, there has been considerable research directed toward the outcomes of the children born as a result of the method. Most recent studies have shown that the rate of birth defects with ICSI is normal compared to IVF and non-IVF pregnancies. Adverse outcomes which have been reported are thought to be related to the population of infertility patients rather than the ICSI process itself. (Palermo, 2017)
ICSI in the future
For purposes of this discussion, we focused on tried and true ICSI methods. New methods to address failed ICSI with chemical activation of the egg are not fully proven. Stay tuned to hear someday about successful use of PLC zeta or other critical components of fertilization in ICSI as IVF research continues.
About BUNDL Blog
The BUNDL Blog features need-to-know information for all aspects of the fertility journey, including info about IVF, IUI, and affording care.