6 Things to Know about Polycystic Ovary Syndrome (PCOS) and Fertility
By Dr. Joe Massey, MD
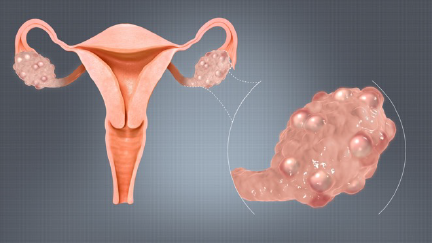
1. Know what PCOS is
Polycystic ovary syndrome is a classification for women who have a variety of symptoms related to menstrual disorders linked to lack of ovulation and resulting failed efforts trying to conceive (TTC). The syndrome revolves around excessive male hormones, known as androgens, being secreted by multiple tiny cysts in the ovaries. The normal monthly cyclic pituitary-ovarian axis of hormonal actions in the ovary is interrupted by the androgens. Thus, ovulation does not occur despite high levels of estrogen.
About 10% of women secrete more than normal amounts of androgens from the ovaries. There are complex faulty signals from the pituitary gland which occur, but the original cause of the endocrine fault lines is not certain. PCOS is definitely hereditary. It is not always found in a family member, but it does follow familial lines.
2. Know the characteristics of PCOS
The number-one symptom of PCOS is skipping periods due to the excess androgens’ interference with ovulation. Other possible causes of skipping periods, such as thyroid disease or other ovulation disorders, are ruled out before making the diagnosis. Irregular ovulation or no ovulation leads to menstrual cycles over 50 days and up to six months apart. Infertility is common as a result.
Other symptoms include:
- Weight gain
- Acne
- Hirsutism (increased hair on the face, chest, and/or abdomen)
- Sugar intolerance due to insulin resistance
The degree to which one woman has these symptoms can vary widely. The hair growth, for example, is increased in brunettes. Their skin has more androgen sensitivity than that of women with light skin and light hair color, who may have no visible hair growth. The varying visible signs of the disorder accounts for differences in opinions among doctors who may be considering the diagnosis. Blood testing can confirm excess androgens to corroborate the suspicion.
All races and ethnicities are at risk for PCOS. The name of the syndrome is based on the findings during surgery many years ago that showed women with obesity, hirsutism and irregular periods had many (poly) ovarian cysts, and the ovaries were enlarged.
Irregular periods
A major component of the diagnosis of polycystic ovarian syndrome is the disturbance of ovulation, which leads to irregular periods. Sometimes these periods can seem to be fairly normal, for example 35 to 40 days, but still anovulatory. More frequently, women with PCOS will have two- to three-month long menstrual cycles and have a few periods a year.
Overweight
Since only approximately half of women with PCOS are overweight, those who are not may be overlooked in terms of early diagnosis. While everyone with polycystic ovaries is not overweight, patients with polycystic ovaries have difficulty metabolizing carbohydrates and they tend to gain weight easily. Putting on pounds may be a constant battle. If there is chronic weight gain, 10 pounds a year can add up rapidly, resulting in obesity.
Although advised that a healthy lifestyle is important, it can be discouraging for patients to consider going on a diet. The medication used with PCOS treatment can help burn carbohydrates and can help with weight control. The good news is that if there is loss of just 10% to 15%, there is measurable benefit in subsequent fertility treatment, so an obese patient is not required to lose all excess weight to have a good outcome.
The most reliable indicator of excess weight is the body mass index, or BMI, which can be calculated according to the person’s height and weight.
Androgen Excess
Hirsutism, or excess hair growth on the face, chest, or abdomen, is a common symptom of PCOS, almost always caused by androgen excess. Medical practitioners can diagnose the slightly elevated testosterone and other male hormones with blood testing.
A woman who has blond hair and is of northern European ancestry may not have any visible excess hair. On the other hand, a woman from the southern Mediterranean area may have thick hair on her face, chest, and/or her abdomen. Hair on arms and legs is not considered to be significant, nor is light, downy hair.
Insulin Resistance
Patients who have PCOS, particularly those who are overweight, have high levels of insulin. “Insulin resistance” describes an abnormal response to insulin in which sugars and other carbohydrates are not metabolized properly. This makes it easy for weight to accumulate and hard to reduce.
But checking the level of insulin in the blood may not tell the entire story. Many physicians consider the use of insulin-sensitizing drugs, such as metformin, to counteract this effect.
3. Know how PCOS is diagnosed
In your reproductive endocrinologist’s office, ultrasound is a key to the diagnosis of PCOS. There may be classic findings such as a “string of pearls” or “Swiss cheese” appearance of the ovaries. These small cysts are the source of the androgens that are so problematic. Each cyst has an egg, but the eggs are not active.
Your physician will assess the signs and symptoms that suggest PCOS, and lab tests of androgen levels may confirm increased levels and rule out adrenal disease. Thyroid and prolactin levels will be checked for other causes of irregular periods while an A1C level will check to make sure the patient is not already diabetic.
4. Know about trying to conceive (TTC)
Can a PCOS patient have a baby without medicine?
Women with PCOS may ovulate a few times a year, and if they have intercourse at the right time, they become pregnant. This may account for people being pregnant for several months without realizing it. Without medical intervention, it’s almost impossible to predict ovulation that might be next week or in two months. Patients with PCOS may find waiting and hoping frustrating. Waiting for Mother Nature with PCOS is not a great plan if patients are skipping periods and TTC—ovulation induction is the approach that will begin to improve the odds of success.
Diet and exercise
Patients with PCOS should eat a healthy diet with modest amounts of carbohydrates. If 10-15% of the overall weight is lost, benefits are noted medically. Setting a reasonable goal for weight loss can begin at the same time as ovulation induction.
Increasing physical exercise is a healthy addition to a regimen of management of PCOS. Every mile of walking is a bonus in the management of the extra weight and the benefits of a healthy lifestyle and weight loss spill over into pregnancy.
Metformin, who needs it?
As one of the major components of polycystic ovary disease, insulin resistance means that carbohydrates or sugars are not metabolized properly. Metformin is an insulin-sensitizing agent that can be helpful in managing this aspect of PCOS. Patients who can tolerate the intestinal side effects may ovulate and lose weight without any other treatment. Medical opinions vary as to whether metformin should be used in all patients or only in selected ones.
A milder insulin sensitizing treatment for PCOS, is Myo-inositol. Various forms of this class of oral medication are available over the counter and may be recommended, if appropriate, as part of the approach to TTC.
5. Know the options if you are TTC
Ovulation induction with oral medication for PCOS
Patients not ovulating frequently can be treated with oral medication. Your medical team may choose either clomiphene (Clomid) or letrozole (Femara). They have different mechanisms of action, but either may enable a woman with PCOS to ovulate. These medications, along with timed intercourse, can be used as a first step in treating infertility. The dose of the drug is often begun low and increased if ovulation does not occur. Some centers have even used both of these drugs together in patients who don’t respond initially.
If pregnancy is not forthcoming fairly quickly with ovulation induction (OI), the odds of success are improved with intrauterine insemination (IUI). This enhanced regimen is termed OI/IUI.
Some doctors limit the number of ovulation induction and IUI cycles, but arbitrary limits are not necessary. A younger woman can continue trying to conceive with ovulation induction and insemination as long as she would like, with reasonable success rates per cycle of around 15%. However, after somewhere between three and six cycles, people usually start having discussions about moving on to IVF, which has a higher success rate in a short period of time.
Ovulation induction with injectable gonadotropins
Ovulation can certainly be induced with these powerful drugs. Multiple pregnancies are so common that this is a risky strategy. The risks and benefits of these drugs in a specific situation must be individualized.
IVF and PCOS
The good news is that most PCOS patients never need IVF. Over time, OI/IUI can lead to success for those who are patient. For PCOS patients who have not conceived with IUI, IVF is the route to highest possibility of achieving a successful pregnancy.
Twins
Patients with PCOS using either IUI or IVF tend to have abundant follicles, and have a higher risk of twins or high-order multiple gestations.
6. Know the long-term medical consequences of PCOS
Because of the insulin resistance, patients with PCOS have a high risk of diabetes in pregnancy and in later life, as well as long-term risk of heart and vascular disease.
Due to long episodes of high estrogen without periods, the endometrium can overdevelop. Endometrial hyperplasia is the term for this, and in extreme cases, can lead to endometrial cancer later in life.
Long-term issues managing PCOS should be taken up with a primary care physician once the patient has delivered a baby.
The PCOS Awareness Association provides information for women who would like to be connected with a community of other women with PCOS.
About BUNDL Blog
The BUNDL Blog features need-to-know information for all aspects of the fertility journey, including info about IVF, IUI, and affording care.